Minimally invasive keyhole brain surgery
Preserving brain function through fibre-sparing access
Modern brain surgery is no longer defined only by what is removed, but by how the brain is entered and protected.
Advances in minimally invasive, fibre-sparing techniques now allow selected deep-seated brain conditions to be treated through carefully planned surgical corridors. The aim is to minimise unnecessary disruption to healthy brain tissue while maintaining surgical effectiveness and preserving neurological function where possible.
Key points at a glance
- A gentle and precise way to reach the brain: Minimally invasive keyhole surgery focuses on reducing disturbance to healthy brain tissue while treating deep brain conditions.
- Fibre-sparing access: Techniques such as BrainPath separate brain fibres rather than cutting through them, helping to preserve important functions like movement, speech, and thinking.
- Careful selection is essential: Not every brain condition is suitable for a minimally invasive approach. A specialist assessment is needed to determine whether this technique is appropriate.
A clinical milestone in Singapore neurosurgery
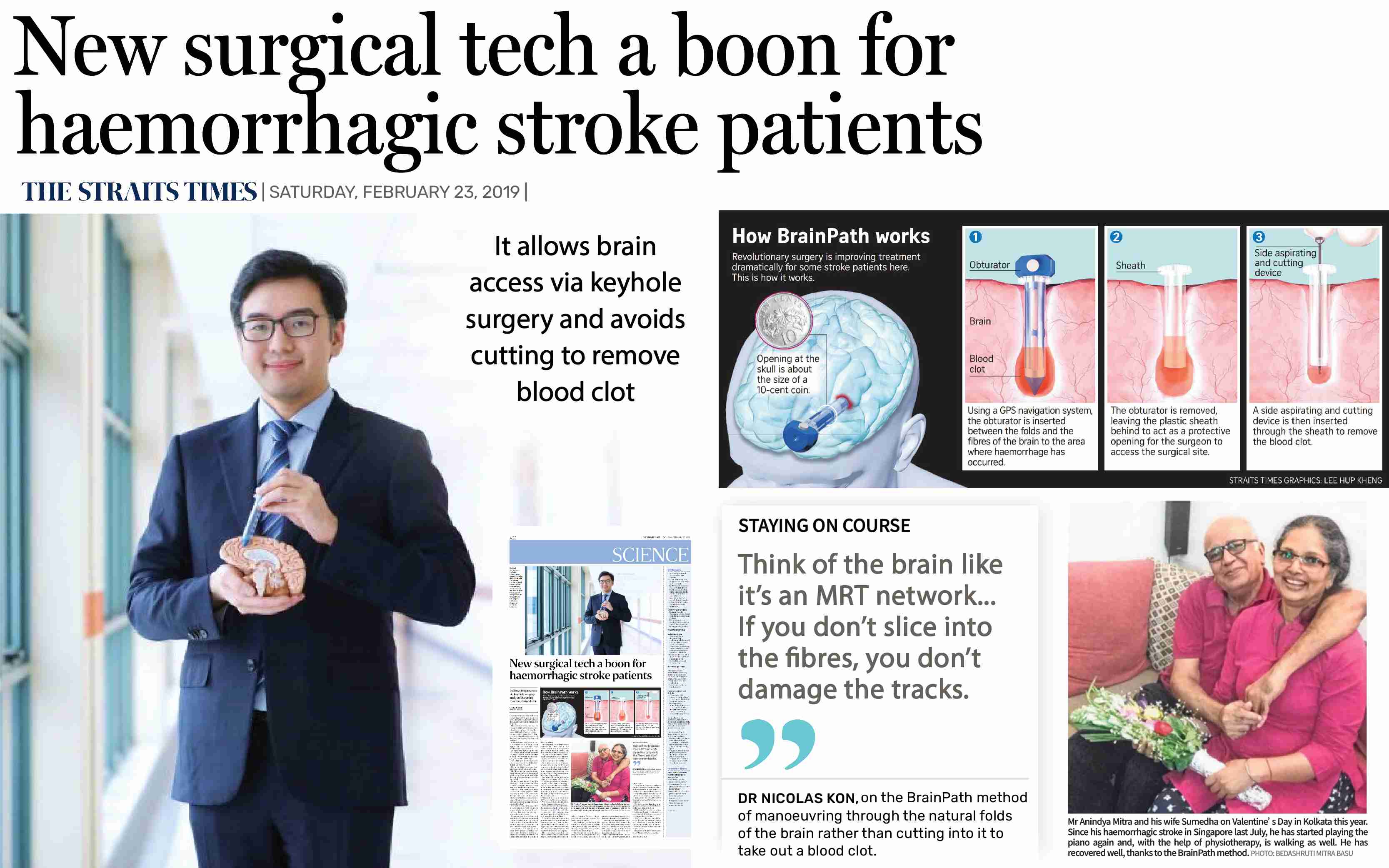
This Straits Times media feature reports on the introduction of the BrainPath minimally invasive brain surgery technique in Singapore, led by Dr Nicolas Kon, senior consultant neurosurgeon in Singapore.
In 2019, Dr Kon applied a fibre-sparing BrainPath approach to remove a life-threatening deep brain blood clot. At the time, conventional surgery would have required significant brain retraction to reach the lesion, increasing the risk of injury to surrounding brain tissue.
This case marked an early milestone in the adoption of minimally disruptive neurosurgical techniques in Singapore, reflecting a broader shift in surgical thinking: from wide exposure of the brain to precise, anatomically respectful access.
Rather than spreading or retracting healthy brain tissue, the BrainPath system allows surgeons to:
- Plan a narrow, targeted surgical corridor through natural brain pathways
- Gently displace surrounding fibres instead of cutting or stretching them
- Reach selected deep-seated lesions with greater control and precision
Today, these principles are applied across a broader range of carefully selected cases including brain tumours and intracerebral haemorrhages, where preservation of neurological function is a key priority.
This page explains the approach in simple terms, outlines its potential benefits, and introduces the expertise behind its use in Singapore.
Why this represents a major advance in brain surgery
Traditional brain surgery focused primarily on removing the disease.
Modern neurosurgery increasingly places equal emphasis on protecting normal brain structure during access.
Fibre-sparing minimally invasive surgery represents an advance because it prioritises:
- Preservation of white-matter pathways. White-matter pathways are the brain’s communication cables that control movement, speech, and thinking. In selected brain tumour cases near areas responsible for speech or movement, this fibre-sparing approach may be combined with awake brain surgery and functional mapping to help protect critical neurological functions.
- Planned surgical corridors, rather than wide exposure or prolonged retraction
- Reduction of collateral injury, where anatomy and pathology allow
As Dr Kon explains:
“Think of the brain like an MRT network.
If you don’t slice into the fibres, you don’t damage the tracks.”
— Dr Nicolas Kon, senior consultant neurosurgeon, Singapore
In simple terms, the goal is to treat the problem while protecting as much normal brain function as possible.
For carefully selected patients, this approach may reduce access-related neurological risks and support smoother early recovery. Outcomes, however, depend on the underlying condition, its location, and individual patient factors. No surgical technique eliminates risk entirely.
Fibre-sparing minimally invasive brain surgery focuses not only on removing the disease, but on preserving normal brain tissue by using carefully planned surgical corridors.
What this may mean for patients
For carefully selected patients, a fibre-sparing approach may:
- Reduce unnecessary disruption to healthy brain tissue during surgery
- Lower the risk of access-related neurological deficits, depending on location
- Support smoother early recovery compared with more disruptive access routes
Potential benefits vary depending on the condition, its location, and individual patient factors. Not every patient will be suitable for this approach.
Who may benefit from fibre-sparing keyhole brain surgery
This approach may be considered when:
- The lesion is deep-seated within the brain
- Critical brain pathways for movement, speech, or sensation are nearby
- A narrow, planned corridor offers less disruption than conventional access
- Preserving neurological function is a key clinical goal
This approach is used in carefully selected brain tumours surgeries and evacuation of intracerebral haemorrhages, depending on tumour type, location, and overall treatment goals.
Who may not be suitable
This technique may not be appropriate when:
- The lesion is large, diffuse, or widespread
- Brain anatomy does not allow a safe fibre-sparing corridor
- Conventional open surgery offers clearer access or better disease control
- Non-surgical options such as observation or radiosurgery are more appropriate
Not all brain conditions benefit from a minimally invasive approach. In some cases, wider exposure remains the safer and more effective option.
Expertise behind the technique in Singapore
Dr Nicolas Kon is a senior consultant neurosurgeon with extensive experience in:
- Minimally invasive keyhole brain surgery
- Fibre-sparing and functional neurosurgery
- Complex brain tumours and brain haemorrhages
He led the introduction of the BrainPath technique in Singapore after specialised training and multidisciplinary collaboration.
Dr Kon practises at Neuro Asia Care and Mount Elizabeth Hospital, caring for patients with complex neurological and neurosurgical conditions. His clinical focus includes minimally invasive keyhole surgery for brain tumours and selected deep brain haemorrhage, with an emphasis on precision, safety, and outcomes that matter to patients and families.
Take-home message
Fibre-sparing minimally invasive keyhole brain surgery represents an evolution in modern neurosurgery that prioritises how the brain is accessed, not only what is removed. Introduced in Singapore in 2019 by neurosurgeon Dr Nicolas Kon, the BrainPath approach enables selected deep-seated brain lesions to be reached through carefully planned corridors that minimise disruption to surrounding white-matter pathways. This technique is applied selectively in certain brain tumours and intracerebral haemorrhages, where preservation of neurological function is a key consideration. Careful patient selection is essential, as not all brain conditions are suitable for minimally disruptive access, and surgical approach decisions are based on anatomy, disease characteristics, and overall safety rather than incision size alone.
When to seek specialist advice
If you or a family member has been diagnosed with a brain tumour or deep brain condition and are exploring treatment options, a specialist neurosurgical consultation can help determine whether a fibre-sparing approach is appropriate.
At Neuro Asia Care, Dr Nicolas Kon provides individualised assessment focused on safety, function preservation, and informed decision-making.